Published On: 27th June, 2024
Authored By: Bhama R
The English and Foreign Languages University, Hyderabad
- ABSTRACT
This article aims to look at the advantages and concerns of AR technology in the field of healthcare. It will also explore how the mechanisms of augmented reality (AR) help in better diagnosis and treatment of diseases by analysing its connection with the innovative technologies brought about by the spread of virtual reality (VR) in healthcare services. The paper focuses on the security requirements of AR healthcare applications and evaluates the efficacy of the Intelligent Security Model proposed by Ara et al in eliminating external threats.
2.KEYWORDS
Augmented Reality, Virtual Reality, Mixed Reality, Intelligent Security Model
3.INTRODUCTION
A technology called augmented reality incorporates digital data into the user’s physical surroundings. It uses elements of Virtual Reality and superimposes them on to the real-world environment in the form of a live video displayed on the screen of an electronic device. AR devices create an illusion of the user’s surroundings enabling them to engage with it in real time using their visual and auditory senses, sometimes even adding an olfactory element to the range of sensations.
The three key components of augmented reality are immersion, presence, and engagement. Depending on the technology being used, immersion can be achieved by head-mounted devices, concave or 3D projections, or user-centric videos. Presence and interaction are related to the individual perception of being connected to the environment and the ability to act within the environment and receive feedback and reaction [1]. In contrast to VR, an AR user always experiences their own reality in real time rather than perceiving the imitation of reality. Azuma et al reported that a VR environment is a completely synthetic environment that separates the user from reality [2].
AR is a relatively new concept; however, it is already being widely discussed in the mainstream of surgery planning and patient treatment in healthcare. The increased stress in public healthcare systems has led to a quick progress in the use and development of AR technologies. But there are a variety of security concerns that make the technology vulnerable to several threats and challenges and reduce its potential in healthcare applications.
4.LITERATURE REVIEW
AR is just an extension of VR. Although the surveys and research evaluating the efficacy of augmented healthcare applications are limited, VR has already been used in healthcare since the last century and its efficiency in the field of medicine is successfully proven. In medical education, VR has been often used for surgical and physical examination skills training, acquisition of anatomical knowledge, and building empathy for patients with neurodegenerative diseases [3]. The use of VR simulators helps in diagnostic and surgical procedures, such as improving novice hospital residents’ laparoscopic skills in terms of error and procedure time reduction. It is also used to assess the suturing skills of different groups of operators. In surgery, it was suggested that VR and simulation could be of value for 4 aspects, namely training and education, surgical planning, image guidance, and telesurgery [1].
Immersive and non-immersive VR have varied applications in healthcare. Non-immersive VR has been used to add cognitive challenges and virtual obstacles to treadmill training for older adults, targeting attention, perception, and dual tasking during walking with the aim to reduce fall risk [4]. On the other hand, the use of immersive VR was beneficial in managing a spectrum of emotional problems, such as the fear of heights, anxiety disorders, depression, and ASD. Immersive VR could also reduce pain in patients, such as those with severe burn injuries during wound care and pediatric patients during invasive medical procedures [1].
Milgram et al used the term Mixed Reality (MR) to distinguish different MR displays and design a taxonomy for categorization of MR systems. It can be explained by the “reality-virtuality continuum”; they anchor one end with a purely real environment, “consisting solely on real objects,” and the other, with a purely virtual environment, “consisting solely of virtual objects”. Mixed reality environments where the real world is augmented with virtual content are called augmented reality (AR), while those where most of the content is virtual but there is some awareness or inclusion of real-world objects are called augmented virtuality (AV). Within this framework, MR can be defined as any display that presents a combination of real and virtual objects that are perceived at the same time [5]. MR has been defined as a stronger version of AR. Nevertheless, in popular culture, the distinction between mixed and augmented reality has been blurred.
MR is defined as the merging of real and virtual worlds and can be seen as a larger class of technologies covering the display environment of AR and AV [6]. Where virtual information augments the real view in AR, real-world information augments the virtual scene in AV. The term of MR was included to embrace new technology labelled as MR, that tries to define a clear distinction between AR and MR, even if there is none [7].
The increasing expectations that AR and MR may be appropriate for healthcare education in various contexts can be explained by their capacities to offer situated and authentic experiences connected with the real environment, enhance interaction between the physical and virtual content, and maintain a feeling of presence. [8].
The recent advancements in augmented reality in healthcare are indicative of their advantages over conventional therapy. It can deliver high-standard and new types of content in highly immersive and realistic ways, remotely, catering to diverse clinical contexts.
Despite all these advancements, a number of challenges hinder us from achieving the entirety of augmented healthcare applications. Ensuring data security is the chief concern in implementing augmented reality in healthcare. Generally, augmented healthcare application provides services through a physical layer with overlaid computer-generated information [9]. Hence it is also subjected to external risks and cyber security risks. This raises the need of a security model that can help prevent threats or network attacks.
5.RESEARCH METHODOLOGY
The primal focus of the research is a literature review followed by the analysis of the security model proposed by Ara et al in 2021 [10]. It addresses a variety of concerns that exploit the vulnerabilities and limitations of AR in healthcare. In order to thoroughly understand the need of a security model, the study would include a basic overview of the distinct AR security and privacy conditions including security requirements and attack terminologies.
As mentioned, the first stage of this study would involve the discussion of security requirements and expected challenges in the successful implementation of AR technology.
The second stage of the study would involve the evaluation of the proposed Intelligent Security Model and its technical aspects in light of the inferences of the first stage and qualitatively analysing its efficacy.
6.RESULTS
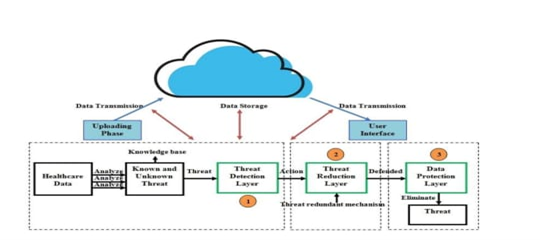
Figure 1 Intelligent Security Model proposed by Ara et al (2021)
Figure 1 presents the Intelligent Security Model for AR-based healthcare solutions proposed by Ara et al in 2021. It operates by following three security layers: threat detection layer, threat reduction layer and data protection layer. Threat detection layer issues directives for action upon detection and notifies threat reduction layer of its observations. Threat reduction layer uses redundant threat mechanisms to fight against threats.
Finally, data protection layer eliminates detected threats and protect the valuable data [10]. The three-layered dynamic security model works as an effective barrier in detecting, reducing and eliminating the threats or attacks that attempt to steal or manipulate data during data transmission or communication.
7.DISCUSSION
Data security and privacy is the primal concern that needs to be addressed while building an AR healthcare application. Ensuring completely encrypted and protected data transferring environment is prerequisite for the application of a safe and secure augmented platform. The second main challenge is to launch a specialized platform that refers to applications package interface (APIs), framework, and appropriate libraries. It helps application designers and developers to manage effective code and classes and implement effective documentation.
Attackers may try to steal data or replace them with unrealistic data and create confusion. Also, false information may get injected to the network which reduce data reliability, affect hardware platform by altering program code, information or reprogramming. Sometimes attack can be introduced through software platforms such as operating systems or software applications and take advantage of software vulnerabilities that cause buffering, resource destruction or loss [10].
Augmented platform should provide security during the collaboration of virtual and real-time object. To provide medical data security, augmented platform should ensure confidentiality which forbids or prevent unregistered access to medical information. That is where the need of a three-layered data protection mechanism arises. Threat detection layer is designed to receive healthcare data from healthcare devices and analyse the captured information to detect the presence of threats. The threat reduction layer is designed to reduce the attack. Data protection layer helps protect data by defending all identified attacks. This security layer performs through dynamic algorithms and provides a shield against the attacks.
However, a handful of challenges concerning the implementation of AR healthcare applications would remain unaddressed in this paper. The high development and implementation cost of the AR healthcare devices, effectiveness of functionalities etc create barriers to increasing the access and acceptability of such devices. The solutions for such challenges are beyond the scope of this paper.
8.CONCLUSION
Realising the full potential of AR technology is an indispensable need of this digital era. The increased stress in public healthcare systems pushes the development and access to AR devices. Hence, the security requirements and concurrent concerns in their application need to be addressed. The proposed security model analysed in this research has found to be effective in addressing some of the challenges particularly in enhancing data security.
9.REFERENCES
- Yeung, A. W. K., Tosevska, A., Klager, E., Eibensteiner, F., Laxar, D., Stoyanov, J., Glisic, M., Zeiner, S., Kulnik, S. T., Crutzen, R., Kimberger, O., Kletecka-Pulker, M., Atanasov, A. G., & Willschke, H. (2021). Virtual and Augmented Reality Applications in Medicine: Analysis of the Scientific Literature. J Med Internet Res, 23(2), e25499. doi: 10.2196/25499. PMID: 33565986; PMCID: PMC7904394.
- Azuma, R. T. (1997). A survey of augmented reality. Presence: Teleoperators & Virtual Environments, 6(4), 355-385.
- Barteit, S., Lanfermann, L., Bärnighausen, T., Neuhann, F., & Beiersmann, C. Augmented, Mixed, and Virtual Reality-Based Head-Mounted Devices for Medical Education: Systematic Review. JMIR Serious Games, 9(3), e29080.
- Mirelman, A., Rochester, L., Maidan, I., Del Din, S., Alcock, L., Nieuwhof, F., Rikkert, M. O., Bloem, B. R., Pelosin, E., Avanzino, L., Abbruzzese, G., Dockx, K., Bekkers, E., Giladi, N., Nieuwboer, A., & Hausdorff, J. M. (2016). Addition of a non-immersive virtual reality component to treadmill training to reduce fall risk in older adults (V-TIME): a randomised controlled trial. The Lancet, 388(10050), 1170–1182.
- Skarbez, R., Smith, M., & Whitton, M. C. (2021). Revisiting Milgram and Kishino’s Reality-Virtuality Continuum. Frontiers in Virtual Reality, 2, 647997.
- Milgram, P., & Kishino, F. (1994). A Taxonomy of Mixed Reality Visual Displays. 77 IEICE Transactions on Information and Systems 1321.
- Brigham, T. J. (2017). Reality Check: Basics of Augmented, Virtual, and Mixed Reality. 36 Med. Ref. Servs. Q. 171.
- Zhu E, Lilienthal A, Shluzas LA, Masiello I, Zary N. (2015). Design of Mobile Augmented Reality in Health Care Education: A Theory-Driven Framework. JMIR Medical Education.
- Daher, S. (2017). Optical see-through vs. Spatial augmented reality simulators for medical applications. In 2017 IEEE Virtual Reality, VR 2017 – Proceedings (pp. 417-418). Article 7892354. IEEE Computer Society.
- Ara, Jinat & Bhuiyan, Hanif & Bhuiyan, Yeasin & Bhyan, Salma & Bhuiyan, Muhammad. (2021). AR-based Modern Healthcare: A Review.