Published On: 27th June, 2024
AUTHORED BY: DR. SIDDIQUA PARVEEN
Abstract:
The classic triad of oedema, proteinuria, and hypoalbuminuria is the usual presentation of nephrotic syndrome. Various researches led to the establishment of nephrotic syndrome in 1830. The causes of nephrotic syndrome were classified into primary and secondary causes. This disease’s assessment is made up of investigations that involve protein, creatinine, albumin, triglycerides, and other tests. In most cases, the treatment involves the use of steroids, antibiotics, diuretics, and immunomodulators. There are various complications associated with steroid therapy so monitoring is important. Further research are on to determine the advanced therapies for nephrotic syndrome.
Keywords:
Nephrotic syndrome, proteinuria, oedema, steroids, diuretics, nephrosis
Introduction:
Nephrotic syndrome (NS) is a clinical syndrome defined by massive proteinuria responsible for hypoalbuminemia, with resulting hyperlipidemia, edema, and various complications.1
It is caused by increased permeability through the damaged basement membrane in the renal glomerulus, especially infectious or thrombo-embolic.2
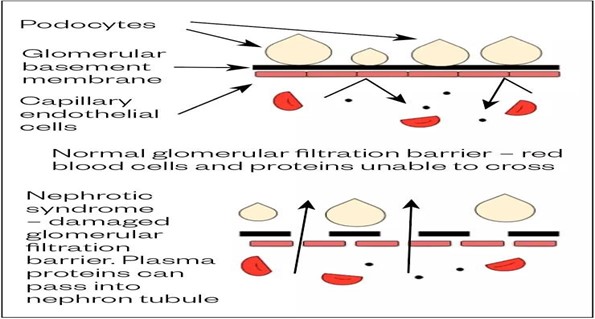
Figure 1:https://pharmaceutical-journal.com/article/ld/nephrotic-syndrome-in-adults- symptoms-and-management
The term “nephrotic-range proteinuria” refers to the loss of three grams or more of proteins through urine in a 24-hour period or the presence of two grams of protein for every gram of urine creatinine in a single spot urine sample. This proteinuria can also result from other systemic diseases, such as amyloidosis.3
In children, nephrotic-range proteinuria is defined by urinary protein excretion rates >40 mg/h per meter.4
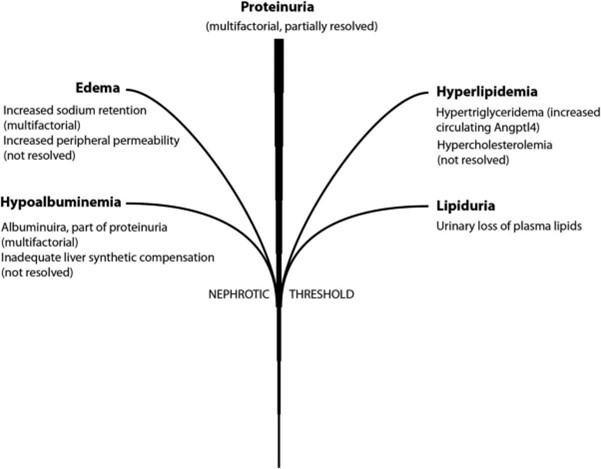
Figure 2: Macé, Camille & Chugh, Simran. (2014). Nephrotic Syndrome: Components, Connections, and Angiopoietin-Like 4-Related Therapeutics. Journal of the American Society of Nephrology: JASN. 25. 10.1681/ASN.2014030267.
History of Nephrotic Syndrome:
Nephrotic syndrome, as we know it today, is a concept that took some time to be developed. It’s interesting to note that efficient treatments weren’t around until the middle of the 20th century, when diuretics, steroids, antibiotics, and other immunomodulators were developed.
Generalized edema, referred to as dropsy in the earlier literature, has been documented from the times of Hippocrates.5,6 One observation by Hippocrates was: “when bubbles settle on the surface of the urine, it indicates a disease of the kidney and that the disease will be protracted”.5 Cornelus Roelans of Belgium described in 1484 a child with nephrotic syndrome and “whole body swelling.” He went on to recommend the treatment as follows: “take the tops of elder plant and daneswort, cook in white wine and wrap the child in hot clothes by applying the poultice in whole or in part, and so cure him”.7
One of the first accurate descriptions of nephrotic syndrome in children was made by Theodore Zwinger of Basel in 1722.8
It was finally in 1827 that Richard Bright (1789–1858) was able to put together the triad of generalized edema, proteinuria, and kidney disease, as presenting features of this disease.9 John Bostock, a colleague of Bright, also noted that when protein in the urine was highest, it was lowest in the serum.9 Christison confirmed these findings in 1829.10 Hence by 1830, nephrotic syndrome of profound albuminuria, hypoalbuminemia, and edema, resulting from diseased kidneys was established.
Latescent or milky appearance of the serum was known to be present in nephrotic syndrome (noted with bloodletting sessions). Christison showed this to be from ether soluble fat.11 Virchow introduced the term “parenchymatous nephritis” for a pathological picture with primary tubular involvement.12
Müller replaced parenchymatous nephritis with the term “nephrosis” in 1905 to refer to all “non-inflammatory” kidney illnesses, but exudative and inflammatory disorders would continue to be called nephritis.13 This concept of “nephritis in contrast to nephrosis” was further popularized by F. Volhard, T. Fahr, and C. Munk.
Epidemiology:
A significant chronic illness that affects children is nephrotic syndrome. Nephrotic syndrome is thought to affect two to seven new instances out of every 100,000 children under the age of eighteen each year in healthy children. At younger ages, it affects boys more frequently than girls.
Increased incidence and more severe diseases are seen in African American and Hispanic populations.14
The most prevalent type of diabetic nephropathy is linked to nephrotic syndrome, with an estimated 50 occurrences per million people.
In the pediatric population, nephrotic syndrome could occur at a rate of 20 cases per million.15
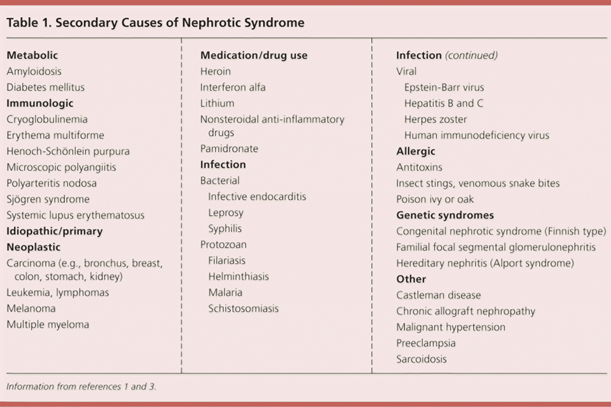
Etiology:
Common primary causes are: Focal segmental glomerulosclerosis, membranous nephropathy, membranoproliferative glomerular disease and minimal change disease
Sources: UpToDate,16 BMJ,17 MSD,18 Am Fam Physician19
{1.Hull RP, Goldsmith DJ. Nephrotic syndrome in adults. BMJ. 2008;336(7654):1185-1189
- Floege J. Introduction to glomerular disease: clinical presentations. In: Johnson RJ, Feehally J, Floege J, eds. Comprehensive Clinical Nephrology. 5th ed. Philadelphia, Pa.: Elsevier Saunders; }
Diagnosis:
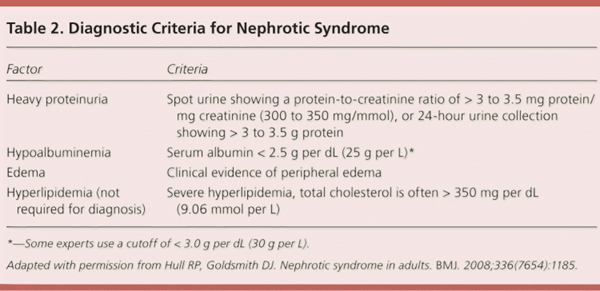
Investigations:20
Urine
- Dipstick: proteinuria 3–4+
- Microscopy: quantify any haematuria – INS may have microscopic haematuria
- spot protein : creatinine ratio >0.2 g/mmol
- sodium <10 mmol/L (consider if concerns about intravascular volume depletion)
Blood
- FBE
- UEC: mild elevation of serum creatinine with mod-severe volume
- LFT
Further diagnostic assessment is aimed at identifying the underlying cause and assessing complications:21
- Thyroid function tests
- vitamin D and calcium levels
- Autoimmune screen
- Virology screen
- HbA1c and fasting glucose
- Serum free light chains or urine protein electrophoresis – may suggest amyloidosis or multiple myleloma
- Renal ultrasound to assess renal size and morphology
- Renal biopsy to determine histologic
Molecular Links between Proteinuria and Other Components of Nephrotic Syndrome:
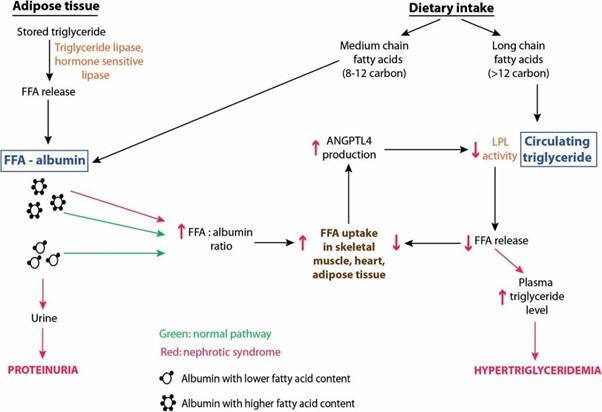
Figure 3:Macé, Camille; Chugh, Sumant S.. Nephrotic Syndrome: Components, Connections, and Angiopoietin-Like 4–Related Therapeutics. Journal of the American Society of Nephrology 25(11):p 2393-2398, November 2014. | DOI: 10.1681/ASN.2014030267
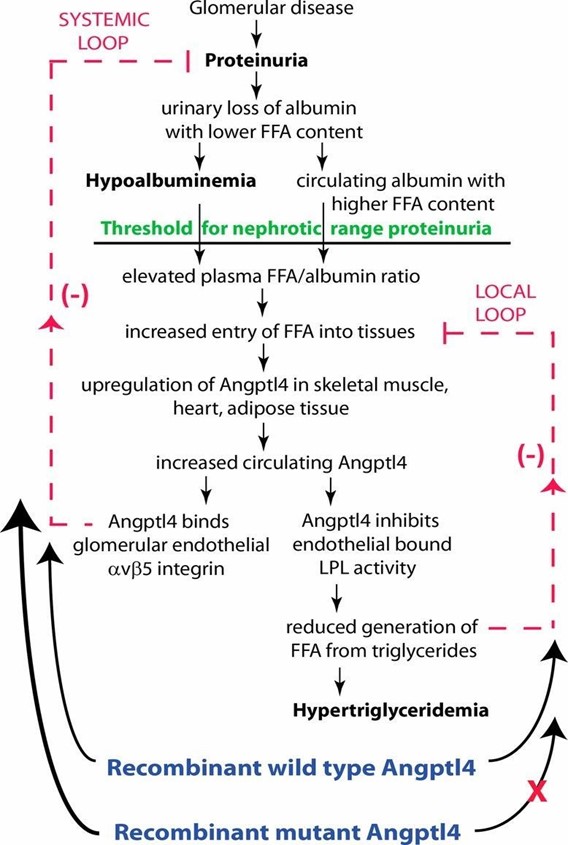
Figure 4:Macé, Camille & Chugh, Simran. (2014). Nephrotic Syndrome: Components, Connections, and Angiopoietin-Like 4-Related Therapeutics. Journal of the American Society of Nephrology : JASN. 25. 10.1681/ASN.2014030267.
Complications:
|
Complications |
Contributing factors |
|
Weight gain |
Secondary to fluid retention |
|
Dyslipidaemia |
Increased hepatic lipoprotein synthesis |
|
Hypothyroidism |
Loss of thyroid-binding globulin |
|
Infection |
Loss of circulating immunoglobulins and complement factors |
|
Thromboembolic event |
Hypercoagulopathy that may be owing to urinary anticoagulant protein losses (e.g. antithrombin, protein C and protein S) and the increased hepatic synthesis of procoagulant factors (e.g. fibrinogen, factor V and factor VIII) |
|
Breathlessness |
May be owing to pulmonary oedema, pleural effusions or a pulmonary embolism |
|
Bone disorders |
Corticosteroid use; vitamin D deficiency owing to loss of vitamin D binding protein |
|
Hypertension |
Owing to renal sodium retention |
|
Renal failure |
May be related to severe active disease or chronic progressive disease process, but can also occur with the use of diuretics if hypovolaemia occurs |
Sources: Am J Med,22 BMJ,17 MSD,18 Am Fam Physician19
Nephrotic syndrome treatment response definitions:
|
Complete remission |
Proteinuria reduced to <0.3g/day or uPCR <300mg/g (<30mg/mmol) with stable plasma creatinine and albumin >35g/L |
|
Partial remission |
Proteinuria reduced to 0.3–<3.5g/day or uPCR 300–<3500mg/g (30– 350mg/mmol) and a reduction of >50% from baseline |
|
Relapse |
Proteinuria >3.5g/day or uPCR >3500mg/g (350mg/mmol) after complete remission previously achieved |
uPCR: Urine protein/creatinine ratio Source: KDIGO 23,24
Treatment algorithm:
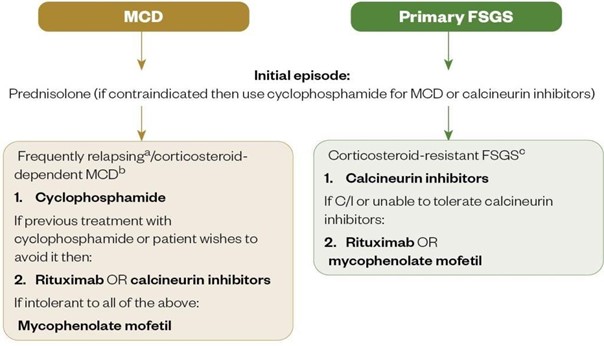
FSGS: focal segmental glomerulosclerosis; MCD: minimal change disease
a: frequently relapsing MCD: ≥2 relapses over a 6-month period (or ≥4 over 12 months)
b: corticosteroid-dependent MCD: relapse during or within 2 weeks of prednisolone completion
c: corticosteroid-resistant FSGS: proteinuria persisting >3.5g/day or uPCR >3500 mg/g (350mg/mmol) with <50% reduction from baseline despite prednisolone treatment for at least 16 weeks
Source: Kidney Disease Improving Global Outcomes 23,24
Treatment (for INS): 20
- Admit to hospital on first presentation
- If the child is profoundly ill or appears to have sepsis treat accordingly
- Manage oedema
- No added salt diet
- Daily weights, daily urine dipstick
- Strict fluid balance with close attention to volume status
Albumin and Furosemide
Indications include: intravascular volume depletion, severe or symptomatic oedema Monitor for hypertension and pulmonary oedema
Albumin: 20% Albumin 5 mL/kg (1 g/kg) over 4 hours IV
Furosemide: 1 mg/kg max 40 mg over 20 minutes IV
- Give mid albumin infusion provided adequate peripheral perfusion
- A second dose may be required at the end of albumin infusion if severe or symptomatic oedema
4. Steroid therapy
- Prednisolone: to induce remission, followed by a slow wean to reduce risk of relapse
- 60 mg/m2/day (max 60 mg) for 4 weeks
- then 40 mg/m2/day (max 40 mg) on alternate days for 4 weeks
- then 20 mg/m2/day on alternate days for 10 days
- then 10 mg/m2/day on alternate days for 10 days
- then 5 mg/m2/day on alternate days for 10 days
- then cease
Body Surface Area (m2) calculator
When calculating maximum doses use pre-morbid weight if known
- Defer live vaccines whilst on high dose steroids
- Prophylaxis against complications
- Infection
- Routine prophylaxis is not indicated unless there is risk of pneumococcal infection
- If indicated, manage with oral penicillin V (phenoxymethylpenicillin) 125 mg/dose 12 hourly if under 5 years, or 250 mg/dose 12 hourly if over 5 years. Cease after oedema subsides
- Gastritis
- Routine use of acid suppressing therapies is not indicated unless there are upper gastrointestinal symptoms while on steroid therapy
Treatment of relapses:
A relapse is defined as proteinuria 3+ or 4+ for 3 consecutive days, and should prompt re- introduction of full dose prednisolone:
- Prednisolone 60 mg/m2/day (max 60 mg) until urine protein is 0, trace or + for 3 consecutive days
- Then weaning regimen:
- 40 mg/m2/day on alternate days for 2 weeks
- 20 mg/m2/day on alternate days for 2 weeks
- 15 mg/m2/day on alternate days for 2 weeks
- 10 mg/m2/day on alternate days for 2 weeks
- 5 mg/m2/day on alternate days for 2 weeks Body Surface Area (m2) calculator
When calculating maximum doses use pre-morbid weight if known
The total time of weaning regimen can be shortened if the child relapses infrequently (2–3 relapses in any 12-month period) and responds to treatment quickly
If oedema recurs, penicillin prophylaxis should also be restarted (see dosing above)
Management of complications:
|
Complications in a nephrotic syndrome |
Prevention strategies |
Monitoring |
|
Proteinuria |
ACE inhibitors (e.g. ramipril, lisinopril) or ARBs (e.g. losartan, candesartan). |
Gradually titrate up to maximum tolerated dose. On discharge, BP and Urea and electrolytes should be monitored every one to two weeks; Risk of hyperkalaemia and acute kidney injury — monitor U&Es as above; Advise patients to monitor for dry, persistent cough from ACE inhibitor (if troublesome, switch to ARB); To minimise first-dose hypotension, take ACE inhibitor at night or split initial dose into twice per day. |
|
Oedema |
Fluid restriction to 1–1.5L/day; Dietary sodium restriction (<100mmol/day, 2g/day); Loop diuretics daily (e.g. intravenous furosemide 80– 120mg/day) initially and titrated as per response. Can step down to oral furosemide or bumetanide. Furosemide requires protein binding to reach its site of action in the renal tubule, which is reduced owing to hypalbuminaemia; |
Monitor weight and fluid balance daily as an inpatient (target weight reduction 0.5–1kg/day). Risk of hypotension, hyponatraemia, hypokalaemia, hypomagnesaemia, alkalosis and acute renal failure if fluid taken off too quickly — close monitoring of daily BP, U&Es and renal function is necessary |
|
|
therefore, higher doses may be required in resistant cases; Plus or minus: thiazide diuretics, potassium-sparing diuretics or metolazone, which can act synergistically; Plus or minus IV albumin (in resistant cases to aid delivery of furosemide to site of action). |
every one to two weeks on discharge until a stable dose is reached; Advise patients to take diuretics in the morning and at lunch (if twice-daily dose) to minimise sleep disturbance from diuresis. |
|
Hyperlipidaemia |
If high cardiovascular risk, lipid- lowering therapy, such as statins/ezetimibe can be initiated |
Lipid profile taken on diagnosis and then every three to six months. |
|
Hypothyroidism |
If thyroid function tests (TFTs) are deranged and patient is symptomatic, option to treat with levothyroxine 50– 100mcg daily in the morning. |
Test TFTs when NS first diagnosed and annually for those who remain nephrotic. |
|
Infection |
Prophylactic antibiotics not advised. |
Patients advised to receive pneumococcal vaccine every five years and yearly influenza vaccines. |
|
Thromboembolism |
If nephrotic range proteinuria and serum albumin <25g/dL, anticoagulation may be considered; Warfarin is the preferred agent or low-molecular-weight heparin could be used as an alternative. |
Regular international normalised ratio (with warfarin); Consider stopping prophylactic anticoagulation if persistent albumin >25g/dL and no other indication to continue. |
Sources: KDIGO,23 KDIGO,24 UpToDate,25 Am Fam Physician,26 Clin Pharmacol
Ther,27 Pharm J,28 Nephrol Dial Transplant,29 Cochrane Database Syst Rev,30 Eur Thyroid J,31 NIDDK32
Management of potential adverse effects from high-dose steroid treatment:
|
Adverse effects |
Management strategy |
|
Pneumocystis pneumonia (PCP) |
PCP prophylaxis with co-trimoxazole 480mg daily or 960mg three times per week; If intolerant or allergic to either component of co- trimoxazole, dapsone 50–100mg daily can be initiated (dose dependent on renal function). |
|
Fungal infections |
prophylaxis with fluconazole 50mg daily. |
|
Risk of gastric ulceration |
Advise patients to take prednisolone with food; Gastroprotection with a PPI or H2 receptor antagonist. |
|
Osteoporosis risk |
Calcium/vitamin D combination supplementation.High-risk patients (e.g. older people or postmenopausal females) should also receive an appropriate bisphosphate (extra consideration of risk/benefit if estimated glomerular filtration rate<30mL/min/1.73m). |
|
Hyperglycaemia |
Pre-meal capillary blood glucose (CBG) monitoring; If CBG>12mmol/L on 2 occasions in 24 hours, gliclazide, or intermediate-acting insulin (Humulin I/Insulatard/Insuman Basal) may be considered;HbA1C;Optimise and titrate doses to maintain CBG’s between 6–10mmol/L. |
Sources: KDIGO,23 Ann Rheum Dis,33 EMC,34 JBDS-IP35
Future Treatments:
It’s interesting to note that ACTH is making a comeback as a possible nephrotic syndrome treatment. It is available as a highly purified formulation (Acthar gel) from pig or cow sources in the US and as a synthetic depot formulation (Synacthen) in Europe.36
New drugs on the horizon, such as losmapimod (p38 MAPK inhibitor), sparsentan (endothelin receptor type 1A antagonist) and biologics such as adalimumab (anti-TNF-α) and abatacept (anti-CD80), hold promise in the treatment of steroid resistant nephrotic syndrome and prevention of renal progression.37
Discharge education:2
- The family should be taught to test urine protein
- After remission, the urine protein should still be checked and documented every day (for at least 1–2 years), in order to identify a relapse at which point the family should contact their treating clinician
- This allows for re-institution of prednisolone prior to the onset of oedema, thus avoiding the associated consequences (admission, risk of sepsis, thrombosis)
- Weight should also be checked daily while nephrotic (as a sign of fluid accumulation)
- It is important to convey that, though their child will likely respond to therapy, they will likely have relapses (80% chance)
- The most common relapse trigger is intercurrent infection. In children on weaning or maintenance alternate day prednisolone, the risk of relapse can be reduced by temporarily increasing the dose from alternate to every day for 3–5 days
Summary:21
- Nephrotic syndrome is a collection of signs and symptoms indicating damage to the glomerular filtration barrier that is characterised by proteinuria (> 3.5g/24 hours), hypoalbuminemia and oedema.
- Treatment involves addressing the underlying cause, as well as taking steps to reduce proteinuria, including an angiotensin-converting-enzyme inhibitor, good blood pressure control and management of oedema via sodium and fluid restriction, and the use of diuretics.
- Further management is aimed at assessing and managing the potential complications of nephrotic syndrome, including the risk of thromboembolism, hypercholesterolaemia and infection.
- Nephrotic syndrome related to primary conditions may require treatment with immunosuppressive therapies under specialist nephrology services.
References:
1.Hill AJ, Stone DE, Elliott JP, Gerkin RD, Ingersoll M, Cook CR. Management of Nephrotic Syndrome in the Pregnant Patient. J Reprod Med. 2016 Nov-Dec;61(11-12):557-
- [PubMed]
2. Raina R, Krishnappa V. An update on LDL apheresis for nephrotic syndrome. Pediatr 2019 Oct;34(10):1655-1669. [PubMed]
3. Tapia C, Bashir StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): May 15, 2022. Nephrotic Syndrome. [PubMed]
4. Clement LC, Liu G, Perez-Torres I, Kanwar YS, Avila-Casado C, Chugh SS: Early changes in gene expression that influence the course of primary glomerular Kidney Int 72: 337–347, 2007
- Chadwick The Medical Works of Hippocrates: A New Translation from the Original Greek (Vol. 174). Oxford: Blackwell (1950) (Section 7, No 34).
- Cameron JS. Five hundred years of the nephrotic syndrome: 1484-1984. Ulster Med J (1985) 54:S5–19.
PubMed Abstract | Google Scholar
- Roelans C. Liber de Aegritudinibus Infantium. München: Verl. der Mu¨nchner Dr. (1484). Google Scholar
- Zwinger T. Anasarca puerorum. In: Basel E, Thurnis JR, editors. Paedioatreia Pract Curationem Puerorumque Morborum Puerilium etc. 5 (1974). p. 659–66.
- Bright R. Reports of Medical Cases. London: Orme (1827). Google Scholar
- Christison Observations on the variety of dropsy which depends on diseased kidney. Edin Med Surg J (1929) 32:262–91.
- Christison On the cause of the milky and whey-like appearances sometimes observed in the blood. Edin Med Surg J (1830) 33:274–80.
- Virchow R. Cellular Pathology as Based upon Physiological and Pathological Histology. Philadelphia: B. Lippincott (1863).
- Müller Morbus Brightii. Verh Dtsch Ges Path (1905) 9:64–99.
- McCloskey O, Maxwell Diagnosis and management of nephrotic syndrome. Practitioner. 2017 Feb;261(1801):11-5. [PubMed]
- Wong W. Idiopathic nephrotic syndrome in New Zealand children, demographic, clinical features, initial management and outcome after twelve-month follow-up: results of a three-year national surveillance J Paediatr Child Health. 2007 May;43(5):337-[PubMed]
- Kelepouris E, Rovin B. Overview of heavy proteinuria and the nephrotic syndrome. 2019.https://www.uptodate.com/contents/overview-of-heavy-proteinuria-and-the- nephrotic-syndrome (accessed Feb 2021).
- Hull RP, Goldsmith DJA. Nephrotic syndrome in adults. BMJ 2008;:1185–9. doi:1136/bmj.39576.709711.80
- Overview of nephrotic syndrome. MSD Manual Professional Edition. https://www.msdmanuals.com/en-gb/professional/genitourinary-disorders/glomerular- disorders/overview-of-nephrotic-syndrome (accessed Feb 2021).
- Kodner C. Diagnosis and Management of Nephrotic Syndrome in Adults. Am Fam Physician 2016;93:479–85.https://www.ncbi.nlm.nih.gov/pubmed/26977832
- https://rch.org.au/clinicalguide/guideline_index/nephrotic_syndrome/#investigations 21.https://pharmaceutical-journal.com/article/ld/nephrotic-syndrome-in-adults-symptoms- and-management
- Kauffmann RH, Veltkamp JJ, Van Tilburg NH, et al. Acquired antithrombin III deficiency and thrombosis in the nephrotic syndrome. The American Journal of Medicine 1978;:607–13. doi:1016/0002-9343(78)90848-3
- Clinical Guidelines for Kidney Disease Improving Global Outcomes. 2012.https://kdigo.org/wp-content/uploads/2017/02/KDIGO-2012-GN-Guideline- English.pdf (accessed Feb 2021).
- Public review draft of the clinical practice guidelines on glomerular diseases. Kidney Disease Improving Global Outcomes. 2020.https://kdigo.org/wp- content/uploads/2017/02/KDIGO-GN-GL-Public-Review-Draft_1-June-2020.pdf (accessed Feb 2021).
- Endocrine dysfunction in the nephrotic UpToDate. 2020.https://www.uptodate.com/contents/endocrine-dysfunction-in-the-nephrotic- syndrome (accessed Feb 2021).
- Kodner C. Nephrotic syndrome in adults: diagnosis and management. Am Fam Physician 2009;80:1129–34.https://www.ncbi.nlm.nih.gov/pubmed/19904897
- Keller E, Hoppe-Seyler G, Schollmeyer Disposition and diuretic effect of furosemide in the nephrotic syndrome. Clin Pharmacol Ther 1982;:442–9. doi:10.1038/clpt.1982.187
- Parker K, Vincent M, Mohammed M, et al. Diuretic therapy explained. The Pharmaceutical Journal. 2015.https://www.pharmaceutical-journal.com/cpd-and- learning/cpd-article/diuretic-therapy-explained/20067545.cpdarticle (accessed Feb 2021).
- Mees EJD. Does it make sense to administer albumin to the patient with nephrotic oedema? Nephrology Dialysis Transplantation 1996;:1224–6. doi:1093/ndt/11.7.1224
- Kong X, Yuan H, Fan J, et al. Lipid-lowering agents for nephrotic syndrome. Cochrane Database of Systematic Reviews Published Online First: 10 December 2013. doi:1002/14651858.cd005425.pub2
- Benvenga S, Vita R, Di Bari F, et al. Do Not Forget Nephrotic Syndrome as a Cause of Increased Requirement of Levothyroxine Replacement Therapy. Eur Thyroid J 2015;:138– doi:10.1159/000381310
- Nephrotic syndrome in National Institute of Diabetes and Digestive and Kidney Diseases. 2014.https://www.niddk.nih.gov/health-information/kidney-disease/nephrotic- syndrome-adults (accessed Feb 2021).
- Park JW, Curtis JR, Moon J, et al. Prophylactic effect of trimethoprim-sulfamethoxazole for pneumocystis pneumonia in patients with rheumatic diseases exposed to prolonged high- dose Ann Rheum Dis 2017;:644–9. doi:10.1136/annrheumdis-2017-211796
- Summary of product characteristics for Electronic Medicines Compendium. 2019.https://www.medicines.org.uk/emc/product/5769/smpc (accessed Feb 2021).
- Management of hyperglycaemia and steroid therapy. Joint British Diabetes Societies for inpatient care. 2014.https://www.diabetes.org.uk/resources-s3/2017- 09/JBDS%20management%20of%20hyperglycaemia%20and%20steriod%20therapy_0.pdf ( accessed Feb 2021).
- Bomback AS, Radhakrishnan Treatment of nephrotic syndrome with adrenocorticotropic hormone (ACTH). Discov Med (2011) 12(63):91–6.
- Gibson KL, Glenn D, Ferris ME. Back to the future: therapies for idiopathic nephrotic Blood Purif (2015) 39(1–3):105–9. doi:10.1159/000368951
PubMed Abstract | CrossRef Full Text | Google Scholar